- Home
-
+
Conditions/Therapies
- Back and Neck Pain
- Facet Injections
- Facet Syndrome
- Failed Back Surgery - FBSS
- Interventional Spine Treatments
- Lumbar and Cervical Epidural Steroid
- Lumbar and Cervical Herniated Discs
- Lumbar and Cervical Radiculopathy (Sciatica)
- Lumbar and Cervical Spinal Stenosis
- Lumbar and Cervical Spondylosis
- Lumbar Disc Syndrome
- Spine Injuries
- Vertebral Compression Fractures
- Numbness and Weakness of Extremities
- Arthritis
- Hand Disorders
- Orthopedic and Sports Injuries
- Achilles Tendonitis
- ACL Injuries
- Ankle Injuries, Rehabilitation
- Arm Pain
- Biceps Tendon Rehabilitation
- Bursa Injections
- Bursitis
- Chondromalacia Patella
- Fibromyalgia
- Frozen Shoulder
- Gait Imbalance
- Golfer's Elbow and Baseball Elbow, Medial Epicondylitis
- Groin Strain
- Headaches
- Hip Injections
- Hip Injuries and Pain
- Impingement Syndrome
- ITB (Iliotibial Band) Syndrome
- Knee Injections
- Knee Injuries
- Labral Tears
- Leg Pain
- MCL Injuries
- Myofascial Pain Syndrome (MPS)
- Neuritis
- Osteoporosis
- Pinched Nerve
- Piriformis Syndrome
- Post-Surgical Rehabilitation
- Rotator Cuff Injuries
- Runner's Knee
- Sacroiliac Dysfunction
- Sciatic Nerve Pain
- Shoulder Injuries
- Snapping Hip | ITB/Iliopsoas
- Tennis Elbow, Lateral Epicondylitis
- TMJ, TMD
- Trigger Point Injections
- Women's Health
- Workplace Injuries
- Other Rehabilitation Services
- Back and Neck Pain
- Meet Dr. Liss
- New Patient Forms
- + News, Blog and Testimonials
- + PRP, Prolo Therapy, Stem
- Massage Therapy
- Acupuncture
- More...
PRP, Platelet Rich Plasma, Prolotherapy, Cellular Regenerative Treatments
New Treatment Options for Pain and Disability
We are very excited to announce a new service within our practice that will further benefit patients with pain and disability. We have decided to incorporate procedures that come under the heading of "Regenerative Medicine" into our practice. We have collaborated with Drs. Gerard Malanga and Jay Bowen of the New Jersey Regenerative Institute to provide Prolotherapy, Platelet Rich Plasma (PRP), and Cellular Regenerative Treatments.

Over our many years of practice, we have treated thousands of patients suffering from musculoskeletal problems with a conservative approach. The vast majority of patients experienced successful treatment with physical therapy, orthotics, medications, corticosteroid injections for acute inflammatory conditions, and hyaluronic acid injections for moderately advanced knee osteoarthritis. Neurosurgical and orthopedic procedures have certainly had a role in improving the quality of life of many of our patients.
However, for a minority of patients, there has been a "treatment gap," where traditional conservative measures have failed to provide adequate relief or improved function, and where surgery is either not an option or not worth the risk.
There is abundant evidence that oral anti-inflammatory medication has significant short-term and long-term side effects. Corticosteroid injections, while effective for acute inflammation, do not address the underlying pathology and are associated with both systemic and local side effects. They do not contribute to healing of tissues and, in fact, are associated with tissue degeneration. Opioids have a role for patients with acute pain, but do not serve a long-term beneficial purpose for the overwhelming majority of patients with subacute and chronic pain. Surgery has made sense for many patients, but is associated with potentially serious morbidity.
According to journals, attended conferences, and closely followed patients, it has become apparent that there is growing evidence in support of three different groups of procedures when utilized in the proper patient population and administered correctly. One of the very attractive features of these treatments is that side effects are extremely rare.
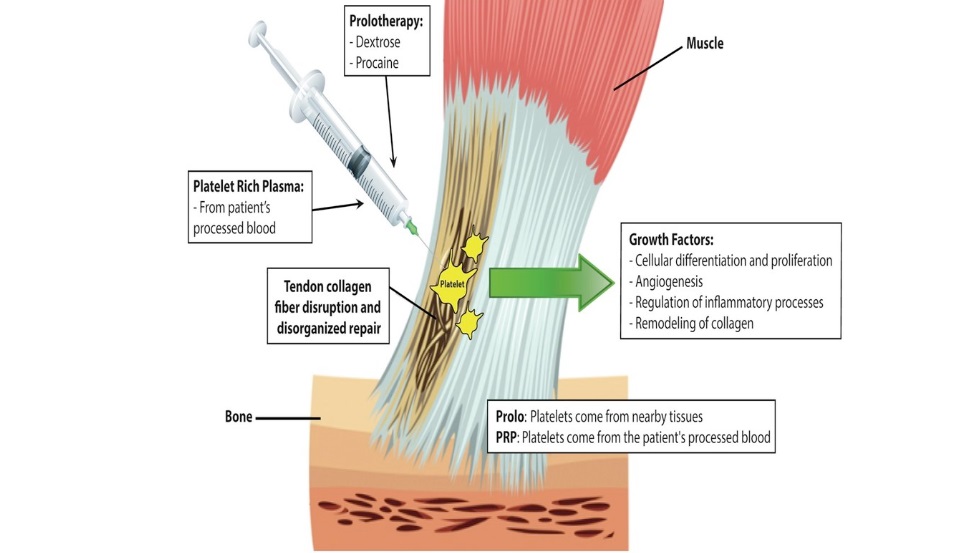
Prolotherapy - prolotherapy has been around since the 1930s and has recently enjoyed an increase in published research. It involves the injection of a solution (commonly dextrose) into tendons and ligaments to stimulate healing in these structures. The injection of the sugar dextrose or other proliferant substances stimulates a reaction that results in greater local blood flow and migration of healing growth factors into the injured tissue. Prolotherapy has been helpful in reducing pain in a number of conditions (knee arthritis, sacroiliac arthritis, and arthritis of the first CMC joint) and tendinitis (tennis and golfer's elbow) (see references).
Platelet Rich Plasma Injections (PRP) - PRP has been around for approximately 20 years but the technique of administration has improved greatly and supportive research has emerged recently. This involves taking the patient's own blood and spinning it down in a centrifuge to produce a medium rich in platelets and growth factors that stimulate healing when injected into injured areas. Often, the involved portions of joints and tendons have poor blood flow, which is felt to be the cause of poor spontaneous healing. This procedure has been shown to be effective with knee arthritis and chronic tendinosis such as rotator cuff tendinitis, tennis and golfer's elbow, and other conditions. (See references).

Cellular Regenerative Treatments - Adipose, BMAC (Stem Cells) - Cellular Regenerative treatments consist of taking a wide variety of cells, including stem cells, from the patient’s own bone marrow and adipose. These growth-factor rich cells are then injected into the area of pain and degeneration. Stem cell injections have been effective in the treatment of arthritis and other conditions. (see references)
I am very fortunate to have entered a collaborative relationship with Drs. Gerard Malanga and Jay Bowen of the New Jersey Regenerative Institute (https://njregenerativeinstitute.com/). Drs. Malanga and Bowen have extensive experience with regenerative medicine, and understand which patient populations and specific conditions have the best chance of responding to the above procedures. In addition, they educate peers, residents, and fellows in procedure and injection techniques.
Dr. Malanga is one of the few leaders in this field internationally. He is triple board certified in Physical Medicine and Rehabilitation (Physiatry), Sports Medicine and Pain Medicine with a fellowship from the Mayo Clinic in Rochester, MN where he remained on the teaching faculty staff for a number of years. Dr. Malanga has co-authored The Atlas of Ultrasound-Guided Musculoskeletal Injections textbook (a comprehensive text on ultrasound guided injections of the Musculoskeletal system) and Regenerative Treatments in Sports and Orthopedic Medicine (the first comprehensive book devoted to orthobiologic treatments for orthopedic conditions written for physicians) as well as contributing regularly to SpineUniverse.com. He was recently elected president of the Interventional Orthopedics Foundation. He lectures internationally on topics within regenerative medicine. His practice includes the treatment of athletes from recreational to the College, Olympic and Professional levels. More can be found at https://njregenerativeinstitute.com/about/gerard-malanga-md.
Dr. Bowen is likewise a leader in the field of regenerative medicine. He and Dr. Malanga have worked closely together for the past 20 years. Dr. Jay Bowen is triple board certified in Physical Medicine and Rehabilitation (Physiatry), Sports and Pain Medicine, and Prolozone Therapy certified. He was the Sports Medicine Fellowship Coordinator at Kessler Institute for Rehabilitation and did his fellowship at UMDNJ-Newark/Kessler Institute for Rehabilitation. He is the medical director of New Jersey Regenerative Institute, LLC. He manages all aspects of pain and performs interventional procedures (ie epidural, facet, sacroiliac joint, etc.). He also delivers medical ozone via various methods (ie systemic HiDose ozone/UBI, insufflation, local injections, etc.). He lectures locally and nationally. Dr. Bowen has and continues to hold various offices for committees such as the Medical Society of New Jersey and the Union County Medical Society. Dr. Bowen was recently appointed to the New Jersey Council on Physical Fitness and Sports in January 2018. More can be found at https://www.njregenerativeinstitute.com/team/jay-e-bowen-do.
I look forward to caring for patients as I always have, and the addition of the above-mentioned procedures will allow for greater success in the management of previously stubborn and resistant conditions.
Sincerely yours,
Howard Liss, MD
Assistant Clinical Professor of Rehabilitation Medicine
Columbia University
Diplomate, American Board of Physical Medicine and Rehabilitation
REFERENCES FOR PROLOTHERAPY, PLATELET RICH PLASMA, CELLULAR REGENERATIVE TREATMENTS
PROLOTHERAPY

Sacroiliac Joint Dysfunction
A randomized controlled trial of intra-articular prolotherapy versus steroid injection for sacroiliac joint pain.
WM Kim, HG Lee, CW Jeong, CM Kim, MH Yoon. Journal of Alternative Complementary Medicine. 2010 Dec;16(12):1285-90
Intra-articular prolotherapy provided significant relief of sacroiliac joint pain, and its effects lasted longer than those of steroid injections.
RTC Tendinopathy
Dextrose Prolotherapy Versus Control Injections in Painful Rotator Cuff Tendinopathy
Bertrand, Helene et al. Archives of Physical Medicine and Rehabilitation , Volume 97 , Issue 1 , 17 - 25
Over the span of 9 months, patients who received dextrose injections were significantly more likely to be satisfied with the results and to have improved pain (59 percent) than patients who received saline injections (27 percent).
Thumb OA
Hypertonic dextrose versus corticosteroid local injection for the treatment of osteoarthritis in the first carpometacarpal joint: a double-blind randomized clinical trial.
A Jahangiri, F R Moghaddam, S Najafi. Journal of Orthopedic Science. 2014 Sep;19(5):737-43
At the end of a 6 month trial, patients treated with 10% dextrose reported significantly better pain and function improvements than the control group.
Knee OA
Dextrose prolotherapy for knee osteoarthritis: a randomized controlled trial.
Rabago D, Patterson JJ, Mundt M, et al. Annals of Family Medicine. 2013;11(3):229-37.
Prolotherapy resulted in clinically meaningful sustained improvement of pain, function, and stiffness scores for knee osteoarthritis compared with blinded saline injections and at-home exercises.
Knee OA
Effect of Regenerative Injection Therapy on Function and Pain in Patients with Knee Osteoarthritis: A Randomized Crossover Study
R Dumais, C Benoit, A Dumais, L Babin, R Bordage, C de Arcos, J Allard, M Bélanger. Pain Medicine, Volume 13, Issue 8, 1 August 2012, Pages 990–999
Prolotherapy is associated with a marked reduction in symptoms, which was sustained for over 24 weeks.
Osgood-Schlatter Disease
Hyperosmolar Dextrose Injection for Recalcitrant Osgood-Schlatter Disease
GA Topol, LA Podesta, KD Reeves, MF Raya, BD Fullerton, H Yeh, PEDIATRICS Volume 128, Number 5, November 2011
Research suggests that dextrose injections are safe, well tolerated, and result in more rapid and frequent achievement of unaltered sport and asymptomatic sport than usual care in the treatment of Osgood-Schlatter Disease in adolescents.
Extensor Tendinosis
The efficacy of prolotherapy for lateral epicondylosis: a pilot study.
M Scarpone, DP Rabago, A Zgierska, G Arbogast, E Snell. Clinical Journal of Sport Medicine. 2008;18(3):248-54.
Prolotherapy with dextrose and sodium morrhuate was well tolerated, effectively decreased elbow pain, and improved strength testing in subjects with refractory lateral epicondylosis compared to Control group injections.
Back Pain
Prolotherapy Injections, Saline Injections, and Exercises for Chronic Low-Back Pain: A Randomized Trial
M Yelland, P Glasziou, N Bogduk, P Schluter, Mary McKernon. Spine. 29(1):9-16, Jan 2004

In chronic nonspecific low-back pain, significant and sustained reductions in pain and disability occur with ligament injections, irrespective of the solution injected or the concurrent use of exercises.
Achilles Tendinosis
Prolotherapy injections and eccentric loading exercises for painful Achilles tendinosis: a randomised trial.
MJ Yelland, KR Sweeting, JA Lyftogt, SK Ng, PA Scuffham, KA Evans. British Journal of Sports Medicine. 2011 Apr;45(5):421-8.
Prolotherapy and particularly eccentric loading exercises (ELE) combined with prolotherapy give more rapid improvements in symptoms than ELE alone but long-term VISA-A scores are similar.
Achilles Tendinosis
Favorable outcomes after sonographically guided intratendinous injection of hyperosmolar dextrose for chronic insertional and midportion achilles tendinosis.
M Ryan, A Wong, J Taunton. American Journal of Roentgenology. 2010;194: 1047-1053.
Dextrose injections appear to present a low-cost and safe treatment alternative with good long-term evidence for reducing pain from pathology at either the insertion or mid portion of the Achilles tendon.
Groin Pain
Regenerative injection of elite athletes with career-altering chronic groin pain who fail conservative treatment: a consecutive case series.
GA Topol, KD Reeves. American Journal of Physical Medicine and Rehabilitation. 2008 Nov;87(11):890-902.
Athletes returned to full elite-level performance in a timely and sustainable manner after regenerative injection therapy using dextrose.
Plantar Fasciosis
Autologous platelet-rich plasma versus dextrose prolotherapy for the treatment of chronic recalcitrant plantar fasciitis.
E Kim, JH Lee, J. H. Physical Medicine and Rehabilitation, (2014) 6: 152-158.
Dextrose and PRP research suggests they are effective for chronic recalcitrant PF, expanding the treatment options for patients in whom conservative care has failed. PRP treatment also may lead to a better initial improvement in function compared with DP treatment.
PLATELET RICH PLASMA (PRP)
Jumper’s Knee
Platelet-rich plasma versus focused shock waves in the treatment of jumper's knee in athletes.
M Vetrano, A Castorina, MC Vulpiani, R Baldini, A Pavan, A Ferretti. American Journal of Sports Medicine. 2013 Apr;41(4):795-803.
Therapeutic injections of PRP lead to better midterm clinical results compared with a shock-wave therapy group in the treatment of jumper's knee in athletes.
Hamstring Strain
Treatment of lateral epicondylitis with platelet-rich plasma, glucocorticoid, or saline: a randomized, double-blind, placebo-controlled trial.
TP Krogh, U Fredberg, K Stengaard-Pedersen, R Christensen, P Jensen, T Ellingsen. American Journal of Sports Medicine. 2013 Mar;41(3):625-35
A single autologous PRP injection combined with a rehabilitation program was significantly more effective in treating hamstring injuries than a rehabilitation program alone.
Lateral Epicondylosis
Treatment of chronic elbow tendinosis with buffered platelet-rich plasma.
A Mishra, T Pavelko. American Journal of Sports Medicine. 2006 Nov;34(11):1774-8.
Treatment of patients with chronic elbow tendinosis with buffered platelet-rich plasma reduced pain significantly in this pilot investigation. Evidence suggests that platelet-rich plasma should be considered before surgical intervention.
Lateral Epicondylosis
Positive effect of an autologous platelet concentrate in lateral epicondylitis in a double-blind randomized controlled trial: platelet-rich plasma versus corticosteroid injection with a 1-year follow-up.
JC Peerbooms, J Sluimer, DJ Bruijn, T Gosens. American Journal of Sports Medicine. 2010 Feb;38(2):255-62
Treatment of patients with chronic lateral epicondylitis with PRP reduces pain and significantly increases function, exceeding the effect of corticosteroid injection. Future decisions for application of the PRP for lateral epicondylitis should be confirmed by further follow-up from this trial.
Knee OA
Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial.
S Patel, MS Dhillon, S Aggarwal, N Marwaha, A Jain. American Journal of Sports Medicine. 2013 Feb;41(2):356-64.
A single dose of WBC-filtered PRP in concentrations of 10 times the normal amount is as effective as 2 injections to alleviate symptoms in early knee OA. The results, however, deteriorate after 6 months. Both groups treated with PRP had better results than did the group injected with saline only.
Hip OA
Ultrasound-Guided Injection of Platelet-Rich Plasma and Hyaluronic Acid, Separately and in Combination, for Hip Osteoarthritis: A Randomized Controlled Study.
D Dallari, C Stagni, N Rani, G Sabbioni, P Pelotti, P Torricelli, M Tschon, G Giavaresi. American Journal of Sports Medicine. 2016 Mar;44(3):664-71.
Results indicate that intra-articular PRP injections offer a significant clinical improvement in patients with hip OA without relevant side effects. The benefit was significantly more stable up to 12 months as compared with the other tested treatments.
Patellar Tendinopathy
Platelet-rich plasma: evidence for the treatment of patellar and Achilles tendinopathy--a systematic review.
B Di Matteo, G Filardo, E Kon, M Marcacci. Musculoskeletal Surgery. 2015 Apr;99(1):1-9.
PRP has been used clinically to treat musculoskeletal pathologies such as Achilles and patellar tendinopathies. This paper reviewed several studies, and concludes that all studies concerning patellar tendon treatments report superior results for PRP than for traditional approaches. For Achilles tendon treatment, clinical data suggests considering PRP as a therapeutic option although more data is encouraged.
Tendinopathy
Platelet-rich plasma in the conservative treatment of painful tendinopathy: a systematic review and meta-analysis of controlled studies.
I Andia, PM Latorre, MC Gomez, N Burgos-Alonso, M Abate, N Maffulli. British Medical Bulletin. 2014 Jun;110(1):99-115.
Pooling pain outcomes over time and across different tendons showed that PRP injections improved pain in the intermediate-long term compared with control interventions
Foot/Ankle
Platelet-rich plasma in the foot and ankle.
PR Henning, BJ Grear. Current Reviews in Musculoskeletal Medicine. 2018 Dec;11(4):616-623.
Recent research has demonstrated platelet-rich plasma to be a promising treatment option for the treatment of Achilles pathology, chronic plantar fasciitis, osteochondral lesions of the talus, ankle osteoarthritis, and diabetic foot ulcers.
Lumbar Muscular Atrophy
Effect of autologous platelet leukocyte rich plasma injections on atrophied lumbar multifidus muscle in low back pain patients with monosegmental degenerative disc disease.
M Hussein, T Hussein. International Society of Orthopaedic Surgery and Traumatology. 2016 Mar 22;2:12.
PRP injections into atrophied lumbar multifidus muscle represent a safe, effective method for relieving chronic low back pain and disability with long-term patient satisfaction and success rate of 71.2%.
Sacroiliac Joint
Steroid vs. Platelet-Rich Plasma in Ultrasound-Guided Sacroiliac Joint Injection for Chronic Low Back Pain.
V Singla, YK Batra, N Bharti, VG Goni, N Marwaha. Pain Practice. 2017 Jul;17(6):782-791.
The efficacy of steroid injection was reduced to only 25% at 3 months treated by steroid, while it was 90% in the PRP group.
Facet Joints
A New Technique for the Treatment of Lumbar Facet Joint Syndrome Using Intra-articular Injection with Autologous Platelet Rich Plasma.
J Wu, Z Du, Y Lv, J Zhang, W Xiong, R Wang, R Liu, G Zhang, Q Liu. Pain Physician. 2016 Nov-Dec;19(8):617-625.
There was a 47% immediate benefit from the PRP injections with 79% benefit at 1 week that lasted to the end of the study at 3 months
Facet Joints
A Prospective Study Comparing Platelet-Rich Plasma and Local Anesthetic (LA)/Corticosteroid in Intra-Articular Injection for the Treatment of Lumbar Facet Joint Syndrome.
J Wu, J Zhou, C Liu, J Zhang, W Xiong, Y Lv, R Liu, R Wang, Z Du, G Zhang, Q Liu. Pain Practice. 2017 Sep;17(7):914-924.
Both PRP and anesthetic/corticosteroid for intra-articular injection are effective, easy, and safe enough in the treatment of lumbar facet joint syndrome. However, PRP is a superior treatment option for longer duration efficacy when compared to the anesthetic/corticosteroid group.
Disc
Intradiscal Platelet-Rich Plasma Injection for Chronic Discogenic Low Back Pain: Preliminary Results from a Prospective Trial.
D Levi, S Horn, S Tyszko, J Levin, C Hecht-Leavitt, E Walko. Pain Medicine. 2016 Jun;17(6):1010-22.
This trial demonstrates encouraging preliminary 6 month findings, using strict categorical success criteria, for intradiscal PRP as a treatment for presumed discogenic low back pain.
Cellular Regenerative Treatments (Adipose and BMAC)
BMAC: bone marrow aspirate concentrate
MSC: mesenchymal stem cells
Osteoarthrosis
Intra-articular Mesenchymal Stem Cell Therapy for the Human Joint: A Systematic Review.
JA McIntyre, IA Jones, B Han, CT Vangsness Jr. American Journal of Sports Medicine. 2018 Dec;46(14):3550-3563.
This review of using MSC therapy in human joints provides strong evidence that the procedure is safe and has generally positive clinical outcomes.
Knee Osteoarthrosis
Clinical efficacy and safety of mesenchymal stem cell transplantation for osteoarthritis treatment: A meta-analysis.
Yubo M, Yanyan L, Li L, Tao S, Bo L, Lin C. PLoS One. 2017;12(4):e0175449. Published 2017 Apr 27.
This article demonstrated that MSC transplantation treatment is safe and has great potential as an efficacious clinical therapy for patient with knee OA. The study looked at numerous clinical and quantitative scales over 24 months to properly observe results of MSC treatment.
Knee OA
A Prospective, Single-Blind, Placebo-Controlled Trial of Bone Marrow Aspirate Concentrate for Knee Osteoarthritis.
Shapiro, S. A., Kazmerchak, S. E., Heckman, M. G., Zubair, A. C., & O’Connor, M. I. (2017). The American Journal of Sports Medicine, 45(1), 82–90.
Early results show that BMAC is safe to use and is a reliable and viable cellular product. Study patients experienced a similar relief of pain in both BMAC- and saline-treated arthritic knees. Further study is required to determine the mechanisms of action, duration of efficacy, optimal frequency of treatments, and regenerative potential.
Knee After Partial Meniscectomy
Adult human mesenchymal stem cells delivered via intra-articular injection to the knee following partial medial meniscectomy: a randomized, double-blind, controlled study.
CT Vangsness Jr, J Farr, J Boyd, DT Dellaero, CR Mills, M LeRoux-Williams.The Journal of Bone and Joint Surgery: American Edition. 2014 Jan 15;96(2):90-8.
There was evidence of meniscus regeneration and improvement in knee pain following treatment with allogeneic human mesenchymal stem cells. These results support the study of human mesenchymal stem cells for the apparent knee-tissue regeneration and protective effects.
Knee OA Adipose Safety
Adipose Mesenchymal Stromal Cell-Based Therapy for Severe Osteoarthritis of the Knee: A Phase I Dose-Escalation Trial.
Pers YM, Rackwitz L, Ferreira R, et al. Stem Cells Translational Medicine. 2016;5(7):847-56.
The study demonstrated that local injection of autologous adipose-derived stem cells was safe and well tolerated in patients with knee osteoarthritis. This study also provides encouraging preliminary evidence of efficacy. Larger and controlled long-term studies are now mandatory to confirm whether this new strategy of cell therapy can improve pain and induce structural benefit in osteoarthritis.
Knee OA – adipose
Intra-articular Injection of Mesenchymal Stem Cells for the Treatment of Osteoarthritis of the Knee: A 2-Year Follow-up Study.
CH Jo, JW Chai, EC Jeong, S Oh, JS Shin, H Shim, KS Yoon. American Journal of Sports Medicine. 2017 Oct;45(12):2774-2783.
This study reported that an intra-articular injection of adipose-derived MSCs improved knee function and reduced pain for up to two years, regardless of the cell dosage of the injection. There were significant improvements in the high dose groups as opposed to the low and medium dose groups.
Proof of concept paper
Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof-of-concept clinical trial.
CH Jo, YG Lee, WH Shin, H Kim, JW Chai, EC Jeong, JE Kim, H Shim, JS Shin, IS Shin, JC Ra, S Oh, KS Yoon. Stem Cells. 2014 May;32(5):1254-66.
The results of this paper showed that intra-articular injections of adipose-derived MSCs into knees with OA improved function and pain without adverse effects. Furthermore, cartilage defects were reduced as a results of cartilage regeneration. The study used numerous clinical and quantitative scales to measure improvement, as well as arthroscopic techniques.
Knee OA – adipose
Clinical results and second-look arthroscopic findings after treatment with adipose-derived stem cells for knee osteoarthritis.
YG Koh, YJ Choi, SK Kwon, YS Kim, JE Yeo. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA. 2015 May;23(5):1308-16.
Adipose-derived stem cell therapy for elderly patients with knee OA was effective in cartilage healing, reducing pain, and improving function. Therefore, adipose-derived stem cell treatment appears to be a good option for OA treatment in elderly patients.
Rotator Cuff – Adipose
Intratendinous Injection of Autologous Adipose Tissue-Derived Mesenchymal Stem Cells for the Treatment of Rotator Cuff Disease: A First-In-Human Trial.
CH Jo, JW Chai, EC Jeong, S Oh, PS Kim, JY Yoon, KS Yoon. Stem Cells. 2018 Sep;36(9):1441-1450.
Shoulder pain was significantly alleviated by 71% in the high-dose group. Magnetic resonance imaging examination showed that volume of the bursal-side defect significantly decreased by 90% in the high-dose group. Arthroscopic examination demonstrated that volume of the articular- and bursal-side defects decreased by 83% and 90% in the mid- and high-dose groups, respectively. Intratendinous injection of adipose tissue derived MSCs in patient with a partial-thickness rotator cuff tear did not cause adverse events, but improved shoulder function, and relieved pain through regeneration of rotator cuff tendon.
Knee OA – adipose
Autologous and micro-fragmented adipose tissue for the treatment of diffuse degenerative knee osteoarthritis.
A Russo, V Condello, V Madonna, M Guerriero, C Zorzi. Journal of experimental orthopedics. 2017 Oct 3;4(1):33.
The results of this study show the safety and feasibility of using autologous and micro-fragmented adipose tissue in patients affected by diffuse degenerative chondral lesions. The technique is safe, minimally invasive, simple, one-step, with low percentage of complications, and compliant with the regulatory panorama.
Disc
Intervertebral disc repair by autologous mesenchymal bone marrow cells: a pilot study.
L Orozco, R Soler, C Morera, M Alberca, A Sánchez, J García-Sancho. Transplantation. 2011 Oct 15;92(7):822-8.
MSC therapy may be a valid alternative treatment for chronic back pain caused by degenerative disc disease. Patients injected with MSCs exhibited rapid improvement of pain and water content, and the results favorably compare to more invasive procedures. This procedure is more advantageous dues to its conservative nature, maintenance of natural tissues and bone, as well as comparable pain relief.
Disc
Percutaneous injection of autologous bone marrow concentrate cells significantly reduces lumbar discogenic pain through 12 months.
KA Pettine KA, MB Murphy, RK Suzuki, TT Sand. Stem Cells. 2015 Jan;33(1):146-56.
Patients in this study received BMAC injections and reported substantial reduction in pain, with those receiving higher doses improving significantly faster than low dose patients. This study demonstrates evidence of safety and feasibility in nonsurgically treating degenerative disc disease with BMC, and indicates an effect of mesenchymal cell concentration on pain reduction.
Disc
Treatment of discogenic back pain with autologous bone marrow concentrate injection with minimum two year follow-up.
K Pettine, R Suzuki, T Sand, M Murphy. International Orthopedics. 2016 Jan;40(1):135-40.
BMAC injections do not cause any complications in patients, and indeed produce encouraging results for the use of BMAC in treating disc disorders. 92% of patients avoided surgery through 12 months post-procedure, and 81% through 24 months. Additionally, patients experienced reduced pain, and the rate of pain reduction was linked to MSC concentration in the injection.
Rehabilitation Institute
111 Dean Drive Suite 1
Tenafly, NJ, 07670
Fax: (201) 871-2214
Rehabilitation Institute
1608 Lemoine Ave Suite 201
Fort Lee, NJ, 07024
Fax: (201) 871-2214
Rehabilitation Institute
3736 Henry Hudson Parkway
Riverdale, NY, 10463
Fax: (201) 871-2214